Cataract Surgery
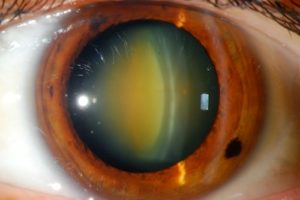
Nuclear Sclerotic Cataract
What is cataract?
Cataract is an opacity in the lens inside the eye that causes some deterioration in vision.This lens does the changing in focussing (accommodation) for seeing up close (eg reading). The lens stiffens with age and cannot change its shape so easily and usually people become aware of this in 40’s or 50’s and have to start wearing reading glasses or switch to multifocals. This is called presbyopia. As this process continues the consistency of the lens changes, interfering with the clarity of vision at all distances, forming a cataract. Once this has occurred the only way to improve vision is with cataract surgery.
What causes cataract?
Cataract is an ageing change in the lens. This happens earlier for some people than others. Genetic factors may play a role and some children are born with cataract. Use of topical or systemic steroids can induce cataract formation. Some intraocular surgery such as vitrectomy can cause cataract and it can also be caused by trauma.
What can you expect from cataract surgery?
Modern cataract surgery is very safe and effective, with most people being extremely happy with the results. You do need to be aware, however, that it is not perfect, despite what you may have heard. Even though we use the most up-to-date technology and lenses there is some variability in the results. In particular, it is not possible to restore the focussing ability of the lens in the eye and make vision perfect at all distances. What this means is that your unaided vision after cataract may not be perfect and it may not be possible for us to make it that good.
We do expect to be able to make you able to function very well in many situations without glasses. Some people will need to wear glasses in some situations, such as for driving at night.
The main issue for most people is what to do about near vision, as explained below.
Many people will know, or will have heard of someone, who has “thrown away their glasses” after having some sort of refractive surgery or cataract surgery. Unfortunately, things are not as simple as that.
What is involved in cataract surgery?
Cataract surgery involves removal of the opacified lens within the eye and its replacement with an artificial intraocular lens (IOL).
This is generally a daycase surgical procedure performed under local anaesthetic with some sedation, though it can be done under general anaesthesia if necessary. Most people find this not too unpleasant and the recovery is usually quick.
The pupil is dilated with eyedrops before the surgery. Three small incisions are made at the edge of the cornea to gain access to the inside of the eye. A circular tear is made in the thin, clear membrane (capsule) that surrounds the lens (a capsulotomy). An ultrasonic probe is then used to liquefy and suck out the cloudy contents of the lens (phacoemulsification). This leaves the thin, clear capsule with a round hole in the front, much like an empty bag.
The replacement intraocular lens (IOL) is made of a soft plastic material that can be folded up and put into a plastic cartridge and then injected through one of the small incisions. It is placed within the capsular bag, where it unfolds. The membrane then gradually shrinkwraps around the lens and holds it in place. This process occurs over several weeks and the focus of the eye takes that long to stabilise.
The incisions in the cornea usually seal themselves and do not require sutures. Antibiotics and steroids are injected around the eye and it is padded closed and protected with a shield until the next day.
With the local anaesthetic there should be no pain involved during the procedure other than some stinging at the start. Usually the anaesthetic affects vision as well and people just see coloured or kaleidoscopic lights during the procedure. A clamp is used to keep the eyelids open. You will be completely covered with a sterile drape and will be lying comfortably on a bed with your head in a rest. You do need to able to lie down flat for this. The procedure takes 15-20 minutes.
For a daycase procedure you will be in the day surgery unit for 3 to 4 hours. Your pupil will be dilated with eyedrops before the surgery. You will stay for an hour or so after the surgery and will need someone to take you home and then to bring you back the next morning to have the eye checked.
What happens after cataract surgery?
Those people with cataracts in both eyes will usually have them done 1 or 2 weeks apart with the worst one done first. You will be using eyedrops for 4 weeks after the surgery and the eyes are checked at 5-6 weeks, when vision should be stable. At that time your refraction is checked and a decision is made about what to do with glasses.
You will be able to see out of the operated eye the day after surgery but vision is usually variably blurry and glarey. Often the pupil is still very dilated. Vision often has a shimmery or flickery quality to start with and many people have some double vision the first morning, which settles down over the day. You will need to be careful on steps and stairs and walking on uneven surfaces. Vision improves day by day for several days and the focus stabilises over several weeks. If you were wearing glasses for distance vision then you may need to have that lens in the glasses removed to use them until the other eye is done.
People often ask how long it will be before they can drive afterwards. This is very variable and depends on many factors and not just how bad the cataract was. It will usually be several days but often longer.
There is some restriction on your activity afterwards but it is not as strict as it used to be with this operation. You can bend down and be active but not do any hard physical activity for a week or so. Light exercise is fine but no swimming for 2 weeks.
Return to work depends largely on what you do. If a lot of computer work is involved that may be difficult until both eyes are done and vision has stabilised but it is mostly a question of how comfortable you are doing it.
Intraocular lenses (IOL’s)
The most important decision with regard to cataract surgery is what sort and what strength of intraocular lens to use as there are several options these days. This decision needs to be made before the operation and it determines what the focus of the eyes will be afterwards. Unfortunately, it is not possible to restore the distance and near focussing of the lens as it was when you were young.The only ways around this issue are compromises of one sort or another. There is no one treatment yet that will restore full focussing ability at all distances for both eyes.
Most people compromise just by wearing glasses for near work or multifocal glasses if they need them for distance as well. Multifocals are a compromise in that they are not as good optically as single vision glasses for any given distance but only one pair is required instead of multiple. In this situation we aim to make distance and general “getting around” vision good in both eyes with monofocal IOL’s.
Some people are comfortable with what is called a monovision correction, where one eye is focussed for distance vision and the other for near vision to some degree. Most people can manage a modified monovision correction with the near vision eye focussed at -1.00 to -1.50, which gives good vision at computer distance and reading vision in bright light. Reading glasses would be required in dim light, for prolonged reading or computer work, for very small print or for very near vision. Not so many people are comfortable with a full monovision correction with the near vision eye focussed around -2.50 allowing good reading vision. This is not so good for computer distance.
The other alternative is to use a bifocal or multifocal intraocular lens. Multifocal lenses have a distance and near focus but have different limitations to bifocal or multifocal glasses. Multifocal IOL’s split up the light coming into the eye so that there is a distance and a near focus (or more). This means that not all of the light is used for each and vision may not be as good in some circumstances. With these lenses most people are aware of some ghosting or haloes around lights at night but this tends to become less noticeable over time. Some people, though, are not happy with the quality of vision with multifocal intraocular lenses in any situation and they have to have them removed and replaced with monofocal lenses.
Newer extended-depth-of-focus (EDOF) lenses give a greater range of focus without technically being multifocal. These work well for many people but there are still some who have issues with quality of vision in some circumstances.
People who have always been short-sighted (myopic) sometimes prefer to keep the ability to see clearly up close and read without glasses. In that case we can choose lenses to keep them short-sighted but they will still need to wear glasses for long distance vision.
There are several ways of dealing with this issue and what suits one person does not necessarily suit another. All those people who have “thrown away their glasses” are accepting a compromise of one sort or another as far as their vision is concerned, whether they are aware of it or not.
Whatever sort of lens is used there is some variability in how the focus ends up after the surgery despite us having very sophisticated measurements to try to predict this. This means that even distance vision without glasses may not be as good as you might expect afterwards in one or both eyes. The variability is greater for those people who are very long-sighted or short-sighted to start with. It may be possible to do something to improve vision without glasses afterwards, such as laser treatment or changing the intraocular lens, but there will be a cost for that and there is an added risk of having more complications with any further intervention.
In general, whatever IOL we put in the eye is going to stay there for the rest of your life. Although they can be changed if there are problems, we prefer not to do that because of the risk of complications and it is not feasible to swap the IOL for something better later on down the track.
Risks and Complications
Cataract surgery is generally very safe but there are multiple potential problems that can occur during or after the surgery even in the best of circumstances. The issues range from those that are a persistent nuisance but may not be fixable to those that can cause blindness.
These include but are not limited to the following:
Intraoperative problems
Posterior capsule tear:
The main concern during the procedure is with the membrane (capsule) around the lens in the eye. We tear a round hole in the front of this to do the surgery but if we tear or make a hole in the back of it then the vitreous gel that fills the back of the eye can come through that and need to be cleared away with a vitrectomy procedure. That can increase the risk of having some of the postoperative problems discussed below. If there is a large defect in the capsule then it may not be possible to implant the sort of intraocular lens that was planned, or it may not be safe to implant a lens at all and that would mean another operation to do that. In that circumstance there is more chance of the focus ending up different from what was expected. That may also be more of an issue if a multifocal lens or a lens to correct astigmatism was planned. It is also possible for some of the hard part of the cataract to fall into the back of the eye. If that happens then another operation would be required to remove that.
Iris damage:
The iris can be damaged during surgery. This is more likely for those men who have been on medication for prostate problems as they make the iris floppy (intraoperative floppy iris syndrome, IFIS).
Corneal damage:
The layer of cells (corneal endothelium) on the back of the cornea (the clear window of the eye at the front) can be damaged during surgery. This is more likely to be a problem for those people who already have abnormalities of the endothelium, most commonly Fuchs corneal endothelial dystrophy. Damage to this layer causes swelling of the cornea that prolongs visual recovery. In severe cases corneal transplantation may be required to correct it.
Anaesthetic problems:
There is a risk of problems with either general (off to sleep) or local anaesthesia (+/- sedation) for cataract surgery. That extends from having more discomfort or a more unpleasant experience than usual at the minor end to more rare extreme problems (including death) from an unusual reaction to anaesthesia regardless of the type. For those having sedation with local anaesthetic there is a concern of waking from a drowsy state and moving during the procedure.
Postoperative problems
Infection:
Infection in the eye (endophthalmitis) can occur with cataract surgery. It is rare these days with all of the precautions we take to avoid it but if it happens can lead to complete loss of vision even with treatment.
Inflammation:
Some people have more inflammation in the eye than usual afterwards. This would make the eye more uncomfortable and light-sensitive as well as delaying visual recovery. We have everybody use anti-inflammatory as well as antibiotic drops afterward but some people need to use more of them or need to use them for longer.
Pain:
The eye may be painful the night of the surgery or the morning after. This may be due to the pressure in the eye being high or from the eye rubbing on the pad before the anaesthetic has worn off. This usually recovers quickly with treatment the following morning. It is very unusual to have persisting pain after the surgery.
Persistent foreign body sensation, irritation, discomfort, watering, or photophobia:
Most people find that recovery from the cataract surgery is quite quick and easy but issues of persistent foreign body sensation, irritation, discomfort or watering are quite common.
Some people have persistent discomfort of some sort that can be an unpleasant nuisance. This may relate to the small incisions that have made to do the operation or to disturbance of the surface of the cornea. Many people with cataract also have degenerative changes affecting the surface of the eye or eyelids which mean that the tears do not lubricate the eye so well. Any surgery may cause enough disturbance to make this a problem when it was not apparent before. That may lead to irritation, light sensitivity, or watering. These problems can be more difficult to deal with than the cataract itself.
Corneal epithelial basement membrane dystrophy is a common, genetically-determined, degenerative condition that affects the surface of the eye. People with this are more likely to have these problems after cataract surgery and may need further intervention. It is sometimes better to do something about this before or during the cataract surgery.
Glare and unwanted light effects (dysphotopsia):
The intraocular lenses that are implanted let nearly all light into the eye and many people find that they need sunglasses much more than they did before the surgery (when the cataract is blocking some of the light getting in).
There are also various “unwanted” light effects such as bright or dark crescents in peripheral vision that can occur after surgery. Much of the time this is temporary but occasionally this can be enough of a nuisance that another operation is required and the IOL may need to be exchanged for another sort.
Retinal detachment:
This may occur even with uncomplicated cataract surgery but is more likely to occur in short-sighted (myopic) people or those with pre-existing retinal problems. This would usually require more surgery to fix it.
Floaters:
Floaters are the visual sensation of something moving in the field of vision due to degeneration of the vitreous gel in the back of the eye. These can start or be more obvious after cataract surgery even when it is completely uncomplicated otherwise. There is usually nothing that can be done to get rid of them though they tend to be less obvious over time.
Posterior capsule opacification:
The “capsule” is the transparent membrane that surrounds the lens with the cataract. We have removed a circle from the front of it during the cataract operation and then implanted the IOL in to the “bag” that remains. Some people will develop crinkling or thickening of the posterior part of that membrane months to years down the track. That then affects vision but this is generally fixed quite easily by making an opening in that part of the membrane with a laser so that vision is just through the implanted lens. This is called a YAG laser posterior capsulotomy, a straightforward procedure done in the clinic.