Keratoconus Management
What is Keratoconus?
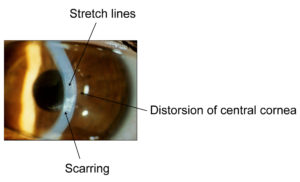
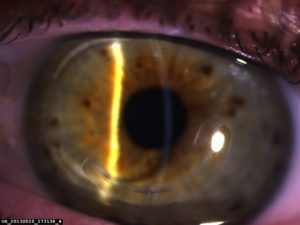
Keratoconus is a degenerative process affecting the cornea, the clear window of the front of the eye, distorting it out of shape and interfering with the focus of the eye. The cornea becomes more conical in shape and this makes vision blurry by making the eye more short-sighted (myopic) and also distorts vision by producing irregular astigmatism (the cornea is not evenly curved). The condition usually affects both eyes but one may be much worse than the other.
Keratoconus is a genetically determined condition but is not necessarily passed on in families. One in twelve people with keratoconus will have an affected relative. If there is not a definite family history then there is a one in ten chance of the children of someone with keratoconus also having it.
Keratoconus is often associated with allergic disorders such as asthma, eczema and hayfever. It is more common in those with Down’s syndrome. It is also more common in people with sleep apnoea syndrome or floppy eyelid syndrome.
What can be done about keratoconus?
There are a number of options for dealing with keratoconus:
Nothing may be necessary in very mild cases or if vision is good in one eye.
Glasses my help if the cornea is not too distorted.
The most helpful option is wearing contact lenses. These will generally need to be rigid gas-permeable (RGP, hard) lenses. This is the quickest way of getting good vision.
If he condition is progressing then Collagen Cross-Linking is advised to stabilise the cornea and prevent further progression.
Intrastromal Corneal Ring Segments (Kerarings) can be used to reduce the distortion of the cornea and improve unaided vision and vision with glasses or contact lenses.
Kerarings
Laser treatment (topography-guided PRK) may be used to further improve vision.
Phakic intraocular lens implantation (phakic IOL, ICL) may be used to reduce high levels of myopia after other procedures have improved vision with glasses.
Corneal transplantation may be required for those who have poor vision even with contact lenses, or who are unable to wear contact lenses.
In young people, or soon after diagnosis, the condition should be monitored for progression.
Can I do anything to prevent it from getting worse?
Unfortunately, there is very little that one can change in daily life or activity that will make a difference to progression of keratoconus. It is known that eye-rubbing makes it worse and this is more likely to be an issue for people with hayfever and allergies. Using anti-inflammatory eyedrops (Cromo-Fresh, Zaditen or Patanol) can help to reduce itching and the need to rub the eyes. Wearing contact lenses does not prevent keratoconus getting worse. If it is getting worse then it is advisable to have collagen cross-linking performed to stabilise it.
Treatment types for Keratoconus
Glasses
Glasses often will not improve vision because keratoconus distorts the shape of the cornea but in milder cases they may be very effective.
Contact lenses
RGP contact lenses work by replacing the smooth and evenly-curved front focussing surface of the cornea. Soft contact lenses usually do not work well in keratoconus because they just adapt to the irregular shape of the cornea underneath. Hybrid contact lenses, combining a soft and rigid lens, are helpful for some people. Contact lens fitting for keratoconus requires skill and experience. You need to see an optometrist who is used to dealing with this.
Collagen cross-linking
When keratoconus is getting worse it is advisable to have collagen cross-linking (CXL) performed to stabilise it.
Layers of collagen fibres make up much of the structure of the cornea. CXL increases the adhesion between collagen fibres in the cornea and makes it stiffer, so that it will not distort so easily (like glueing the pages of a magazine together). It may reduce the amount of distortion and improve vision in some cases but this is unpredictable and the main aim is to prevent it getting worse. It does not make vision better in most cases and there is a small risk of it being worse after the procedure. Rarely, CXL needs to be repeated to stop progression of the keratoconus.
CXL involves removal of the corneal epithelium and then soaking a yellow dye (riboflavin) into the cornea using eyedrops. The cornea is then irradiated with an ultraviolet light for 10-30 minutes. The procedure is performed with local anaesthetic eyedrops and takes about an hour. A bandage contact lens is placed in the eye and usually left for a week until the surface heals. It is sore and light sensitive for at least a week. Vision will usually be worse initially and improves over weeks. It takes months for most of the effect to occur and it continues to change slowly for more than a year.
It is not known what long term effects this will have on the cornea. Cross-linking may be combined with topography-guided laser treatment or with intrastromal corneal ring segments to try to fix the cornea in a better shape but the best way to combine these is not yet known.
It is important to be very clear that the idea of this procedure by itself is to stop the keratoconus progressing and not to improve vision, though it may do this for some people. If keratoconus is not getting worse then cross-linking is not necessary unless laser treatment is going to be performed.
Intrastromal Corneal Ring Segments (KeraRings or INTACS)
Intrastromal corneal ring segment insertion (ISCRS) involves placing curved pieces of inert plastic into the cornea to make the shape more even. This may improve the quality of unaided vision or allow people to get back to being able to have reasonable vision with glasses or contact lenses. KeraRings, Ferrara Rings and INTACS are different brand names of these ring segments.
ISCRS is also performed with local anaesthetic as a day case procedure. A laser is used to create a ring-shaped channel within the cornea. One or two ring segments are then inserted into this channel. A bandage contact lens is placed in the eye just until the next day. There is some mild discomfort and light sensitivity for a few days. Usually, 2-3 days off work would be required. Vision is changed immediately but the focus continues to change and stabilise up to 3 months after surgery.
ISCRS does not work if the cornea is too thin and distorted. The results are somewhat unpredictable and it improves vision more for some people than others. Adjustments may be required to the position of the ring segments or size or shape of the segments. Long term results or effects on the cornea are not known. It does not preclude having a corneal transplant later, if necessary.
Laser treatment (Topography-guided PRK)
Topography-guided photo refractive keratectomy (tPRK) may be used to improve improve unaided vision or to improve vision with glasses or contact lenses when the cornea is not too distorted or too thin. This needs to be done after, or in combination with, cross-linking to prevent the cornea warning more out of shape as it makes the cornea thinner.
PRK is performed as a day case procedure under local anaesthetic. It involves removal of the corneal epithelium and then a brief laser treatment to change the shape of the cornea. A bandage lens is placed on the eye to protect it and reduce discomfort but it is still quite painful and light sensitive for several days afterward. The initial recovery takes 1-2 weeks and that time would be required off work for most people. Full recovery and improvement takes at least 3 months.
Phakic Intraocular lens implantation
Phakic intraocular lens implantation (Phakic IOL, ICL) can reduce high levels of myopia and reduce the need for contact lenses or thick glasses when the quality of vision has already been improved by intrastromal ring segments or tPRK. This is an intraocular procedure with the risks associated with that.
More information:
See the Keratoconus Association website: www.keratoconus.asn.au
Other sites:
National Keratoconus Foundation (USA): www.nkcf.org
Wikipedia: http://en.wikipedia.org/wiki/Keratoconus