Recurrent corneal epithelial erosions
Recurrent corneal epithelial erosion (corneal epithelial instability)
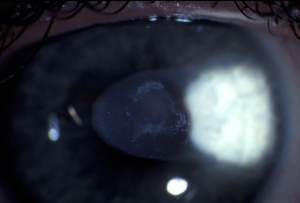
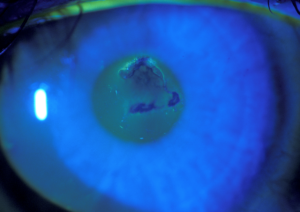
The surface covering of the cornea (the clear window at the front of the eye) is called the epithelium. This consists of 5 layers of cells similar to the skin covering the rest of your body. The epithelium should be firmly adherent to the layer beneath it to maintain stable and clear vision.
In some circumstances the epithelium becomes unstable and can be dislodged by minor trauma or even by friction from the eyelids. This can cause pain, sensitivity to light, and watering of the eye because the cornea is exquisitely sensitive in order to protect itself from injury. Often the symptoms will occur during the night, or on waking, as fewer tears are produced while sleeping and there is more friction from the eyelids. If the affected area is in centre of the cornea then vision may be blurry or distorted.
There are several possible causes of this problem:
Trauma:
Typically this occurs with superficial corneal abrasions caused by fingernails, paper, or other relatively minor injuries. The abrasion may heal over initially but the new epithelium may not stick down as it should and it later lifts off, producing the recurring symptoms of pain or foreign body sensation, and watering, typically on waking. This can happen some time (weeks to months) after the initial injury and persist for years.
Corneal epithelial basement membrane dystrophy (EBMD):
This is a genetically-determined condition that becomes apparent with ageing, in which the adhesion of the epithelium is compromised by abnormal material deposited beneath it. Signs of this may be visible on examination. This condition may affect vision if the abnormal material is in the central, visual part of the cornea. It predisposes to susceptibility to minor trauma.
Blepharitis:
Chronic inflammation of the eyelids and conjunctiva releases inflammatory chemicals into the tear film and these can interfere with corneal epithelial adhesion.
Diabetes:
In the long term diabetes causes a slow increase in thickness of the layer beneath the epithelium and reduces the normal adhesion.
Other corneal dystrophies:
There are a number of uncommon, genetically determined, conditions that can affect the front part of the cornea and predispose to recurrent erosions.
Ageing:
Non-specific degenerative changes in the cornea can reduce epithelial adhesion.
What can be done about it?
There are a number of treatment options:
Reduce friction – use of ocular lubricants:
Using one of the thicker ocular lubricating products before going to bed can reduce friction from the eyelids. This will often alleviate the problem but will not cure it. Non-preserved gels such as PolyGel, or ViscoTears SDU (not the Viscotears in a tube) or with a disappearing preservative (Genteal Gel, Refresh Liquigel) are best. Thicker ointments can be used if the gel does not seem to last long enough (VitAPos, Polyvisc, Ircal, Refresh NightTime). Different people prefer different products as they all feel a little different in the eye.
Thinner drops are better to use during the day, if necessary, as they disturb the vision less.
Treatment of blepharitis:
Even if blepharitis is not the only apparent cause of the problem it helps to control this. Several modes of treatment may be used, including:
- Eyelid hygiene measures (Sterilid), heat and massage on the eyelids
- Steroid (anti-inflammatory) drops or ointment for short-term treatment
- Tears Again/Optrex Actimist Lipid Sprays
- Doxycycline or minocycline tablets may be used for 3 to 6 months
- Omega-3 supplements (fish oil and flaxseed oil, or Lacritec, 3 capsules daily) may also be beneficial in the longer run.
Matrix metalloproteinase (MMP) inhibition:
Enzymes called MMP’s are active underneath the corneal epithelium and they can interfere with the processes required to stick the epithelium down. Inhibiting those enzymes can help control the problem. Steroid eyedrops may be used for weeks to months and doxycycline tablets may be used for months, or even indefinitely, to achieve this. Doxycycline is an antibiotic but it has a completely separate effect at low doses that inhibits MMP’s. Long term use of the steroid eyedrops may cause glaucoma or cataract, though, and needs to be monitored.
Surgical options:
Epithelial debridement:
Once the epithelium is very loose it will often not adhere with any treatment. In that case it is better to remove it and allow fresh epithelium to grow over the defect, The new epithelium has a better chance of adhering.
Anterior stromal puncture:
This procedure involves making very shallow punctures through the epithelium with a needle (after the cornea is anaesthetised). These punctures stimulate a healing response that promotes adhesion of the epithelium. It is easy to do at an outpatient visit and can be repeated if necessary. It does cause pain afterwards, lasting a day or two, and measures need to be taken to deal with that. It is more effective for the localised forms of corneal epithelial instability and does not work so well for those with EBMD.
Diamond burr keratectomy:
Use of a fine diamond burr over the layer underneath the epithelium after debriding it promotes adhesion. It is a more extensive procedure and generally done with local anaesthetic as a formal procedure in the operating theatre.
Excimer laser phototherapeutic keratectomy (PTK):
PTK involves the use of an excimer laser to remove the very superficial part of the layer underneath the epithelium after debriding it. This provides a fresh surface for the epithelium to grow over and adhere to.
Alcohol delamination:
Diluted alcohol can be used to separate the abnormal epithelium from the cornea in an even layer. The new epithelium has a better chance of adhering to the fresh surface beneath this.
Please note that any of the surgical procedures involving epithelial debridement cause pain and disturbance of vision for some time afterwards.
The more extensive the procedure, the worse this will be. If most of the epithelium is removed it will take up to a week to grow back to cover the defect. The new epithelium will then take weeks to months to smooth out and return vision to normal. The process of adhesion takes longer than this – generally 3 months or so. It is typical for patients to have intermittent discomfort or variability of vision during this time.
You will have to expect to be off work or out of action for 1-2 weeks after any of these procedures.
None of the procedures mentioned is 100% effective and they generally work 80-90% of the time, i.e. 8 or 9 out of 10 times. For those that fail the procedure may need to be repeated, or one of the other procedures used. All of the surgical interventions are best used in conjunction with the conservative measures of lubrication, treatment of blepharitis, and MMP inhibition.
More information:
http://en.wikipedia.org/wiki/Recurrent_corneal_erosion
http://www.expert-reviews.com/doi/abs/10.1586/17469899.3.3.253